Near golden sands north of Newcastle, hundreds of people with intellectual disabilities live at the Stockton Centre. Now it's set to be sold to developers. Does the government's new group home model really offer a better future, or is it just a grab for cash?
By Gail Bell
6 December 2017
Reading time: 20 minutes

MY FATHER WAS the youngest of four brothers, a truth he learned at the age of ten. Until this revelation he had counted his older brother Charles as his only sibling. There were reasons for withholding this information, reasons deemed to be the privilege of adults who knew better and who acted in the best interests of young minds.
But old secrets are leaky vessels, prone to barnacles, and gaps that let in water. The news of the existence of other brothers arrived when my father was being warned about how to behave during a rare visit by his father: this man can’t be trusted, he was told, terrible things happened to your other brothers.
I wrote a book, The Poison Principle, about this untrustworthy man who allegedly sinned against his own sons and in the search for facts about two little boys who had been airbrushed from history I came upon the story of Thomas, the firstborn. Stepping into this boy’s story was like opening a door into a room largely unknown to me—an unsettling place to someone with no experience—the room where the less fortunate among us sit out their days.
It is hard to know how to address people who inhabit these rooms in 2017. Are they handicapped, disabled, challenged? Or are they just people with problems that are harder to live with than most? In living history, people with disabilities have been unfairly burdened by the labels stamped on their case notes. Take my father’s brother, for instance.
In 1926 Thomas, aged four, was taken by train to Newcastle, north of Sydney, where he was admitted under the Lunacy Act to a Hospital for the Insane. His record of admission makes harrowing reading. The admitting officer has written of his general appearance “frail thin crippled idiot”. He is stunted, has a small skull, his extremities are paralysed and one side of his face is frozen. He shows no sign of intelligence, does not speak, and has spasms in his limbs when he tries to move. The seventh cranial nerve is mentioned. Trauma at birth is given as the physiogenic cause. Under “supposed cause of insanity” are the initials CMD, or congenital mental deficiency. His mother had stated for the record that she was 18 years old at the time of Thomas’ birth, that it was a long, difficult labour with no doctor present, and that at nine months of age her son could not sit or eat food like other babies, and was “very cross at nights”.
Thomas spent the next seven years at Watt Street Mental Hospital, Newcastle, by all accounts a grim institution designated as an Asylum for Idiots and Weak-Minded Children, a name that was later changed to Newcastle Psychiatric Centre and finally to James Fletcher Hospital. Aged eleven, he was transferred to Peat Island on the Hawkesbury River, then to Milson Island where he died aged twelve from pneumonia. By this time his parents had divorced, the letters written by his mother asking about his welfare had petered out, and the lies about his fate had become accepted truths.*
Questions dangle like untidy threads from this summary of a young person’s life. Why was a child who was traumatised during birth designated a lunatic, for instance? Who made decisions about his welfare after admission? What precipitated his removal to Peat Island, then further upriver to Milson Island where he died just eleven months later?
I put some of these questions to Alfred Taylor OAM, a retired educator and reformer who was seconded to work at Peat Island in the 1960s. We met in his unit in a retirement village on the Brisbane Water, West Gosford, and spoke over coffee.
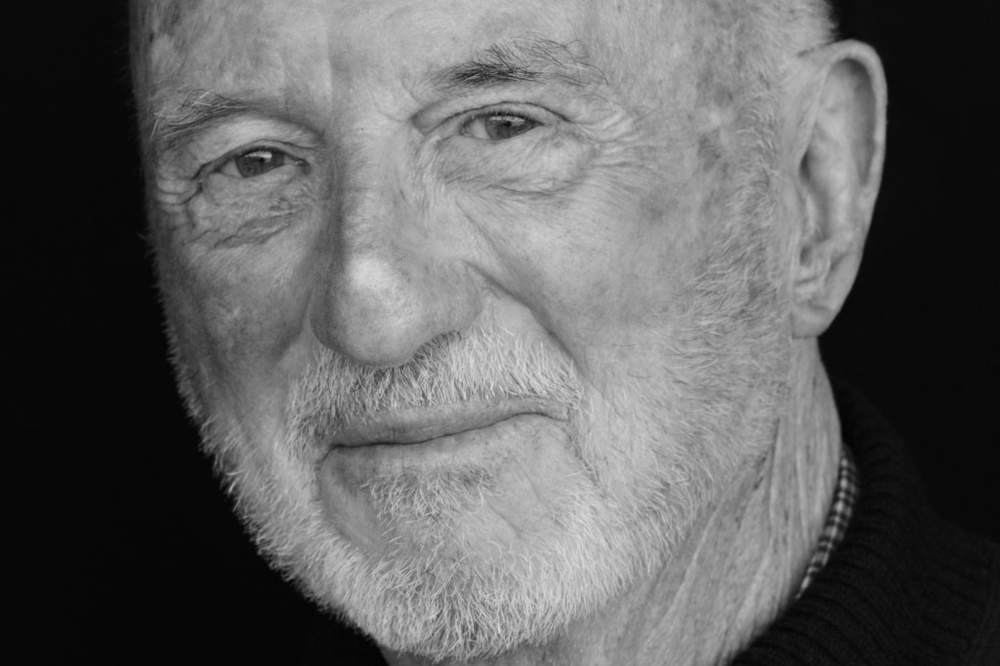
Alfred Taylor OAM
“Well, first of all we had a Master in Lunacy in the very early days. People with mental retardation, as they were called then, were lumped in with psychiatric patients until the late 1950s, early 60s when there was a move to change the prevailing model for people in institutions.” Taylor saw immediately that nurses were the key to that change. In consultation with the newly appointed Director of Mental Retardation, work commenced on a purpose-designed curriculum for nurses in a new speciality called Mental Retardation Nursing, as distinct from Psychiatric nursing. In 1963, Taylor assumed the role of curriculum coordinator. Taylor’s programs extended to Stockton Hospital and other psychiatric institutions, like Callan park, Morriset, Broughton Hall—facilities that had a significant proportion of mental retardation patients. His first question on the job was: “Can we do something special in our institutions? For instance, take over a complete ward and set it up for mental retardation nursing?”
Taylor was on Peat Island for five years overseeing his plan to give patients (all male) the best possible chance for a rounded life. “There were some people on Peat and other institutions who should not have been there. Later on (in 1983) Richmond, in his report, was right in that regard. These wrongly assigned people needed to be resurfaced. I can think of one case of a young boy who had disgraced his family in some way and they’d put him away. He should never have been there.” But this boy was an exception, the majority of Peat Island residents in the 1960s were severely handicapped, with IQs too low to assess. The worst cases went to Milson Island.

“If a child could benefit from something, anything, we made it available to them.”

Taylor lectured to new trainees, and to psych-trained nurses gaining a second certificate in mental retardation training. “Over time we had a variety of programs up and running. Reading and writing, social days, self-care, dancing, cooking, and most importantly a home-like atmosphere with nurses assigned. There were bus trips, even bushwalks, we involved families. Severe cases had diversion and entertainment brought to the ward. If a child could benefit from something, anything, we made it available to them.”
On the whole, Taylor believes that the Richmond Report undid a lot of the good work of community building in an institutionalised setting.
Peat Island was decommissioned in 2010 and its remaining residents assigned to group homes at Wadalba (the Wyong area of NSW’s Central Coast). Taylor has regrets about this: “What we created was a wonderful thing. Living in the broader community is alright for some but there will always be a core of profoundly needy people who are happier and better cared for in a dedicated facility.”
“The transition to group homes needs to be handled better,” Taylor argues. Attitudes of the Not in My Backyard kind, he believes, can be countered with orientation programs. As an educator he advocates involvement: “speak to the neighbours, give clear explanations, lay out the positives and negatives, get them thinking, be part of their awakening.”
THE MOVE TOWARDS what is called “devolution”, or the closure of residential centres like Peat island and now Stockton (scheduled for June 2018), has been driven by strong external forces, notably the Disability Services Act 1993 and more recently the Disability Inclusion Act 2014. But the kick-starter was the much cited Richmond Report of 1983, an enquiry into health services for the Psychiatrically Ill and Developmentally Disabled. Richmond’s reforms sought to change the dominant hospital-based model of care and also the culture of those providing that care.
Thirty years on, the author, David Richmond AO, has written of the report: “Contrary to the misconceptions of some, a significant exodus from institutional care through bed number reductions had already occurred in the 1960s and 1970s, well before the report, largely to meet budget pressure on the institutions.”
Reading this I was reminded of a story a colleague told me in the late 1970s. Her uncle, who had been institutionalised from a young age, had been released into the wider world with a small suitcase of clothes and bus fare. This elderly man who had never previously negotiated a space beyond the walls of his dormitory stood bewildered and afraid on a corner waiting for his nurse to tell him what to do. He stood on the corner for four hours as speeding cars went by and pedestrians stared until someone called the police.
In the past, badly managed first-exits from congregate care have often gone unremarked, mainly due to a lack of advocates with a public voice. Looking back on the net effect of his report, David Richmond has written: “More than thirty years later, despite numerous ‘pockets’ of excellent service, mental health is still underfunded and continues to be locked into hospital care, albeit on a smaller scale…” while “ service provision … appears still largely provider driven when compared with client and family priorities.”

Peat Island on the Hawkesbury River, NSW (Photo: Hpeterswald, Wikimedia Commons)
In March 2007 Australia signed the United Nations Convention on the Rights of Persons with Disabilities (CRPD), with formal ratification on 17 July 2008. This human rights instrument adopted a broad categorization of persons with all types of disabilities and reaffirmed that all “must enjoy all human rights and fundamental freedoms” (my italics). Australia’s declaration recognizes fully supported or substituted decision-making arrangements, that is, decisions made of behalf of a person with disability, “only where such arrangements are necessary, as a last resort and subject to safeguards.”
In 2012 the NSW Department of Family and Community Services or FACS, took another look at the NSW disability laws, enlisting the contributions of over 600 different individuals and organisations, to arrive at a “real change in attitude” with legislation that “gives us a vision of a civilised community with inclusive neighbourhoods but also a framework for removing barriers affecting people in everyday life.” Out of this nexus of consultation with people with disabilities, families, carers, key stakeholders, providers and advocates came the Disability Inclusion Act 2014, with its two broad aims: to set out how FACS will provide disability services until the National Disability Insurance Scheme, NDIS, is rolled out in mid-2018; and secondly, to make sure that after the NDIS has taken over, mainstream services will be available to persons with disabilities and that NSW will make sure that persons with disabilities are “part of the community”.
At this point, slightly numbed by policy statements, acronyms, focus groups and a lot of words on paper, I made an appointment to meet with members of the Stockton Welfare Association, a group opposing the privatisation of the Stockton community. In a recent letter to the Member for Port Stephens, the Welfare Association President, Lorraine Yudaeff, laid out her “real fears about the chaotic planning for the wholesale move to community” of three Hunter-based large residencies, the Stockton, Kanangra and Tomaree Centres. I’d been struck by the passionate and informed tone of her letter and the precise way she contrasted the commitment of policymakers with the reality on the ground. For instance, the commitment that families would have an input into the design of the group home, to ensure that their relative’s needs would be met. The reality facing one particular family was a photograph of the house plan and another of the façade. A simple Google search showed that the house they’d agreed to “backed onto a busy and noisy railway line”, exactly the kind of place their relative could come to harm.

Lorraine Yudaeff (Photo: Jonathan Carroll)
The reality gap seemed widest in the case of a wheelchair bound, frail, deaf and blind person being “reclassified” as not requiring a nurse, when the commitment guarantees trained nursing staff for severely disabled and extremely vulnerable residents.
I met Ms Yudaeff and members of the Association in a conference room at the Stockton Centre, outside the boomgate restricting access to the residential facility. It was my first visit to this area and I was immediately struck by the natural beauty of the Centre’s location. Situated to the north of Newcastle, Stockton peninsula is wrapped by the Hunter River on one side and 32 kilometres of Stockton Beach (facing the Pacific Ocean) on the other. The isthmus is a significant place for the local Aboriginal people of the Worimi Nation, Burrabihngarn being the Worimi name for Stockton.
As far back as 1910 there has been a focus on the importance of the natural environment on the wellbeing of Stockton patients. The evolving “look and feel” of the Stockton Centre, from its earliest days as a quarantine station on land described by early surveyors as a “sandy quagmire covered in thick scrub” to its current outdoor charm, has been steered by the principles of a nineteenth century concept called moral therapy. Under moral therapy principles, architecture and landscaping were fashioned to promote free, open air life in a well-ordered, calming atmosphere (in the thinking of the day, an impoverished social environment was thought to be the cause of physical and mental disorders). Looking around at the generous green spaces and feeling the brush of a nor’easter on my face, I felt a certain affinity with this concept.

“Patients with family at least have someone outside—once I’m dead, what then? It haunts me. I can’t sleep.”

I also entertained the cynical view that this government-owned site would make a handsome golf resort for a billionaire with an eye to the proximity of the golden sands of Stockton Beach (a view that turned out to be not too far off the mark, according to local gossip).
Inside a spacious room with trestle tables forming a U and a small kitchen where an urn was on the boil, I met the group. My visit had been facilitated by the vice president, Wendy Cuneo, who had vetted me with the practised eye of a security chief. Reporters in the past have jumped on this hot button issue and exploited access to the site to produce media stories that play up the “old days” when institutions were likened to Dickensian torture chambers or versions of One Flew over the Cuckoo’s Nest.
Over morning tea supplied by the site kitchen, I turned on my digital recorder. What follows are highlights from nearly three hours of listening to stories that, at times, brought me close to tears.
Wendy’s son David is very active. “Doors don’t mean anything to him.” One thing Stockton has is a lot of green space, over 80 hectares of lawn shaded by Norfolk pines. For David, it is a place to burn off energy, to explore. “Now he’ll be locked inside a group home with people he doesn’t know,” says Wendy, “For patients with family, at least they have someone outside looking in—once I’m dead, what then? It haunts me. I can’t sleep.”

Wendy Cuneo and son David (Photo: Ryan Osland)
Greg’s brother, Neil, has a backstory uncannily close to that of my father’s brother. After a difficult birth Neil suffered irreparable brain damage. The family lived in country NSW with no access to specialised help and by the time Neil was five the difficult decision was made to take him to Newcastle’s Watt Street Mental Hospital.
“Watt Street was a hell hole in those days. We brought him here to Stockton fifty years ago and this is his home.”
Bob and Shirley’s son Wayne is a happy young man who takes an interest in his appearance. I was shown a photograph of Wayne in a tailored suit provided by the family. “It’s the last resort to take [a child] out of the family home,” said Bob. “But Wayne wouldn’t have had the life he’s had, and neither would we, if we’d kept him at home. Here they have activities.” Bob became emotional in the telling and was consoled by his wife and daughter.
I asked Wayne’s sister, Kay, whether the family had a say in her brother’s fate when Stockton closes. “Yes we did. Wayne will go to Blacksmiths (a coastal suburb between Belmont and Swansea). One cottage of four boys is moving together, which is very good for Wayne. But remember, Wayne is in his thirties. What worries us is what the group home will look like in thirty years’ time?” Another concern is not knowing the new staff, and, in terms of potential dangers, not knowing the environment. “Moving is traumatic,” Kay says. “I don’t think the government gives a damn. There’s no long term future planning.”

“The government is acting as if these are the last disability people ever to be born. There’s a new wave coming through; what are they going to do with them?”

Admissions to Stockton were frozen in the early 1990s. Today, as the residents age, those that make up the remaining cohort have a severe intellectual disability, and or a physical disability, and some have challenging behaviours. Smaller, home-style accommodation has been built, cottages, individual bedrooms with more privacy.
“At the end of thirty years the group homes will be past their use-by date,” Lorraine Yudaeff adds. “Within ten years the group houses which are currently rented will be sold to developers. The government is acting as if these are the last disability people ever to be born. There’s a new wave coming through; what are they going to do with them?”
Overseeing the recent deaths in group homes is the office of the Ombudsman for Disabilities. Wendy believes that experience with disability (not public servants shuffling paper in an office) is a pre-requisite for external parties charged with judging the effectiveness or otherwise of existing facilities.
To my question, “What is going to have to happen to make the government get the picture?” the answer comes “They don’t want to. The Minister came up here with some politicians, spent two minutes and said sorry that’s all too confronting and they went away.”
“Other countries have tried the group home solution and it hasn’t worked. People end up homeless or worse, why doesn’t Australia learn from the mistakes of others?”
READING THROUGH THE 2015 Moving Ahead Study led by the School of Social Work and Social Policy, Trinity College Dublin, it is clear that the policy aims of relocating residents to group homes (better services, integration into wider community) are not playing out in the real world. “Despite … the widespread adoption of international rights instruments and national policies, deinstitutionalisation is not enjoying speedy and smooth advances”. After 80 pages of analysis, the study concludes that community living is better than institutional living, but only when support staff is properly trained and accountable.
In Australia, as group home living enters its first decade since the closure of Peat Island, worrying reports are appearing in the media. The ABC television program Lateline recently presented the story of Jason who “died” (and was revived) three times after a serious sepsis, the result of incompatible psychotropic drugs combined in his medication pre-pack. The term “chemical restraint” was voiced, which is to say dosing a person with stupefying drugs in place of physical restraint or the better option, active support. In response, FACS said that the extra medication claim “was inconsistent with what was reported by staff.”
The Moving Ahead study notes that the voices of people with disabilities “though clearly paramount, are rarely reported.” Given that many people with disabilities fail to recognise the side effects of medication, Jason’s case makes a compelling point for properly trained support staff. When asked about his group home, Jason said “I don’t like it. I don’t like the staff.”
One voice that speaks clearly and eloquently for the rights of the disabled is Rosemary Kayess, human rights lawyer and reform advocate. Kayess sustained a serious spinal injury in her twenties and is confined to a wheelchair.

“When people’s behaviour changes, it’s generally their environment they are trying to adapt to.”

Kayess is seeking a Royal Commission into the reported mistreatment of people living in group homes. In her reply to questions put to her on the Lateline program, she said “addressing these incidents through policy is not going to get to the true level and the depth and the cause of these incidents.” She advocates better investigative powers, with officers going into group homes (where, currently there are no spot-checks) to inspect the facilities and assess the group dynamics. “When people’s behaviour changes…and is of concern, it’s generally their environment they are trying to adapt to, an environment that is not conducive to them.” Kayess and others have drawn attention to the growing realisation that group homes are simply smaller versions of an institution. “People don’t get to choose with whom they live, they don’t get to choose who the people are that work around them and are engaged with them sometimes quite intimately and quite personally in their lives.”
She views chemical restraint as a form of mistreatment, a way of trying to resolve behaviours that may in fact be manifestations of a disabled person’s unheard cry for help in a foreign and unsuitable new environment. “There are national standards around what can happen in group homes and …residential services, but there is no holistic approach across the board.”
WITH STOCKTON PROPOSED for closure in June 2018, the question of what will be lost does not seem to have been addressed at policy level. A visit to the Save Our Stockton Facebook page quickly answers that question. Over the past 30 years this group has been constantly active in fundraising, in providing advocacy for residents who have no one to speak on their behalf, and in creating outreach opportunities like the foster grandparent scheme and a buddies program.
Foster grandparents (modelled on a scheme at Kew Cottages in Victoria) are volunteer senior citizens who take an interest in a particular resident, perhaps take them shopping or for walks in the grounds, even bringing them to their own homes for Christmas Day. Currently there are about 50 volunteers. Buddies are volunteers who meet the needs of residents who are “more active”, even hyperactive, with physical activities like swimming (Stockton has its own swimming pool), having a bit of fun in a jumping castle, and ball games.
At Stockton Centre all medical, dental and pharmacy issues are dealt with inhouse. When medications change, as is the case frequently with long-term residents, the onsite GP oversees and organises a new medication pack. Wendy asks: “Who will go to the chemist from the group home? RNs (registered nurses) only go in to do a dressing or a PEG [tube] feed. You’ll have staff trained to the level of certificate 3 or 4, with no background in intellectual disability, doing it, so you’re going to get a lot of wrong meds, dehydration and pneumonias.”

There is an understandable degree of scepticism in the minds of Stockton’s friends towards the lofty sentiments of those in power.

The Association is also about new choices for people with disabilities. In a draft proposal the members have set out a plan for a state-owned, centrally located hub located on the existing Stockton site, a centre of excellence for training and professional development, with room for respite accommodation and, of course, a home for their own residents as well as access for people with disabilities from the wider community who find health services hard to access.
Six months out from Stockton’s proposed closure there is an understandable degree of scepticism in the minds of Stockton’s friends towards the lofty sentiments of those in power. It is their family members who will soon put the theory to the test.
I hark back to the voices I recorded for this story.
Alf Taylor, educator: “If a child could benefit from something, anything, we made it available to them.”
Wendy Cuneo, mother and activist: “Once I’m dead, what then? It haunts me. I can’t sleep.”
And Lorraine Yudaeff, psychologist and activist, whose quiet comment was caught against background noise on my recorder “What’s missing from all this [top down policy making] is love.”
NINETY YEARS AGO, my father’s brother, severely handicapped, voiceless, a misshapen boy in a wheelchair, was swept up and forgotten in the old institutional system. He had no say in his Peat Island placement, or any advocate to plead for him. This is a fundamental right now enshrined in the United Nations CRPD and for this, as a society, we must be grateful.
Peat Island remains in a rezoning limbo. The CEO of Property NSW made this comment in March 2017. “This is prime waterfront location on the edge of the Hawkesbury and is the gateway to the Central Coast, yet much of the land remains dormant, under utilised or inaccessible to the public.”
The NSW Planning Department is considering a proposal for a tourist precinct, marina, neighbourhood hub and 270 new homes. No doubt the speculators have their eyes on 83 hectares of prime land at Stockton, adjacent to Stockton Beach.
Editor's note: Alfred Taylor OAM passed away in late October 2017, several months after he was interviewed for this story. Alf was remembered at his funeral as a pioneering educator. He remained keen for this story to be told.




