When my partner had an anaphylactic reaction at dinner, I realised none of us really knew what to do next. It was supposed to be a normal night out at a new restaurant. We'd taken all the right precautions: mentioned severe allergies when booking and reminded staff on arrival about my partner's anaphylaxis to cashews and pistachios. Toward the end of our meal, we ordered another dish. My partner felt a burning sensation and asked if the dish was spicy. It wasn't. When we approached the manager to check, we found out the dish was loaded with pistachios.
My partner always carries two EpiPens because he understands the risks of dining out. But when it came time to call emergency services, I didn't know how to explain what was happening. The restaurant manager didn't either. So while going through anaphylactic shock and surrounded by capable people, my partner had to make the call himself.
So what is anaphylaxis and how is it different to an allergy?
A food allergy is an immune system reaction that can cause hives, swollen airways and digestive problems. Anaphylaxis, however, is a severe, potentially life-threatening allergic reaction. The Mayo Clinic describes it as causing the immune system to release chemicals that send the body into shock. Symptoms include dropping blood pressure, skin rash and narrowed airways that block breathing. Critically, if anaphylaxis isn't treated immediately, it can be fatal.
There's no cure for anaphylaxis. The only immediate treatment is an epinephrine autoinjector (EpiPen), which delivers adrenaline. However, contrary to what TV shows depict, this isn't an instant fix – 20% of people need a second dose, making hospital monitoring essential.
Managing Allergens: What Restaurants Can Do:
The restaurant where my partner had his reaction put it down to miscommunication during a shift change. Human error happens, but inexperienced staff are more likely to struggle and make mistakes in stressful situations. With allergies and intolerances becoming more common, restaurants need to adapt and accommodate a variety of dietary needs.
Matias Cilloniz, Executive Chef at RAFI, a Sydney based restaurant and bar, explains that understanding allergies and maintaining vigilance is the whole team's responsibility, not just the chefs'. "From that starting point, we design menus with allergens in mind, looking at every component through a dietary lens. Where we can make a substitution without compromising flavour or technique, we do it early in the process. If there's a dish that just isn't naturally adaptable, we balance it out at menu level rather than forcing something that doesn't work. That way we protect creativity and inclusivity at the same time."
For restaurants with flexible menus, a dietary matrix is a useful training tool. It breaks down dishes by ingredients and their sources, plus possible substitutions. Front-of-house staff can access this information, and it's shared during menu planning, so kitchen and service teams can communicate well and advise guests with confidence.
“In our restaurant, when an order with dietary needs comes through, it triggers alerts across sections, prompting an immediate conversation about what needs adjusting”, shares Cillōniz. “Those dishes go out first to avoid confusion and are usually delivered by the manager who will check with the table to confirm the modifications are correct, while ensuring the guests feel included in the experience”.
But what about cross-contamination?
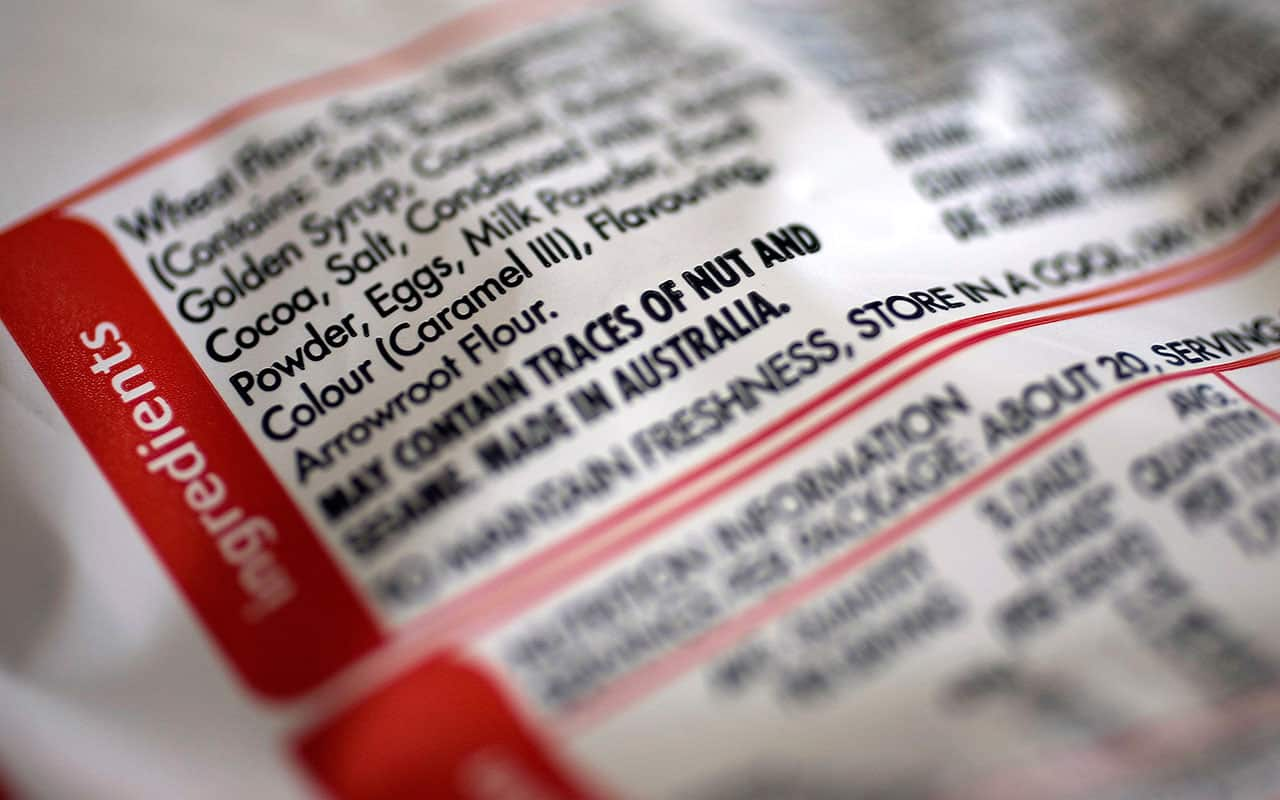
Cross-contamination is often overlooked especially when staff lack proper training. A server might not be aware that a nut-free dish was cooked in peanut oil, or that a dessert comes from a supplier who processes multiple allergens in the same facility. Many restaurants now outsource items like bread, condiments, and desserts, making it tricky to trace what happens during production. When these limitations exist, being transparent with diners from the start becomes essential.
So what should you do if someone has an anaphylactic reaction?
Allergy & Anaphylaxis Australia recommends that all food service professionals take one of the free All About Allergens courses offered by the National Allergy Council. These courses are specifically tailored to different food service settings. Just as Responsible Service of Alcohol certification is mandatory, allergen awareness training equips your staff to identify common allergens, understand cross-contamination risks, and respond appropriately to guest inquiries.
“Keep this phrase front of mind: always ask, always tell,” says Sarah Emery, CEO of Allergy & Anaphylaxis Australia. It’s imperative that waitstaff always ask customers if they have a food allergy, and for those living with allergies to feel that they can make them known without fear of not being taken seriously.“
"If you see someone experiencing anaphylaxis, follow the steps on their ASCIA Action Plan if they have one with them. If not, it's critical to lay the person flat (don't let them stand or walk) and administer an adrenaline device if available. Call an ambulance and give another adrenaline device after five minutes if their symptoms are worsening. Start CPR at any time if they're unresponsive or not breathing normally. If in doubt, always give the adrenaline device. It could save their life. The other important thing to apply to any emergency situation: try to stay calm, stay with the person, and reassure them that help is on the way. If you can call a family member or emergency contact, do so right away" explains Emery.
Understanding the bigger picture
According to the Centre for Food Allergy Research, approximately 2 million Australians live with food allergies, contributing to Australia's unwanted title as the world's allergy capital.
What's particularly interesting is that children born outside of Australia show significantly lower allergy rates. This is likely due to early diet and bacterial exposure. The cultural distinction highlights how food and environment can influence childhood health. Children from Asian backgrounds, for instance, are typically exposed to foods like nuts earlier in life. There's a compelling case for similar approaches in Australia, with a recent LEAP study showing a 70% reduction in peanut allergies following regular exposure in infancy.
In our situtation, my partner has lived with severe allergies for years. He knows the warning signs, carries EpiPens, and understands the risks of dining out. But not everyone with food allergies has that experience or preparedness. Some might be newly diagnosed, not recognise symptoms quickly enough, or not have their medication on hand.
Regardless of prevention strategies, understanding anaphylaxis and its severity is an essential first step. While reducing life-threatening reactions is the ultimate goal, it's just as important to treat diners with allergies with respect, care and compassion. This might mean going the extra mile to accommodate them safely, or it might mean being honest and transparent when you can't. Either way, it's about prioritising their well-being and creating a dining culture where everyone feels truly looked after.
Visit foodallergytraining.org.au to find out more about The National Allergy Council’s online training and allergyfacts.org.au for Allergy & Anaphylaxis Australia’s consumer resources on eating out with food allergy.
SBS Food is a 24/7 foodie channel for all Australians, with a focus on simple, authentic and everyday food inspiration from cultures everywhere. NSW stream only. Read more about SBS Food
Have a story or comment? Contact Us

