Feature
The world is running out of antibiotics. New research could make old ones work again
Australian research could be key to combating the rising threat of antibiotic resistance and saving millions of lives.
Published
The rise of antibiotic resistance is threatening millions of lives worldwide, but "unconventional" Australian research could make obsolete medications effective again.
Data released by the World Health Organization (WHO) has found that some of the most common illnesses in the world are becoming more resistant to treatment every year.
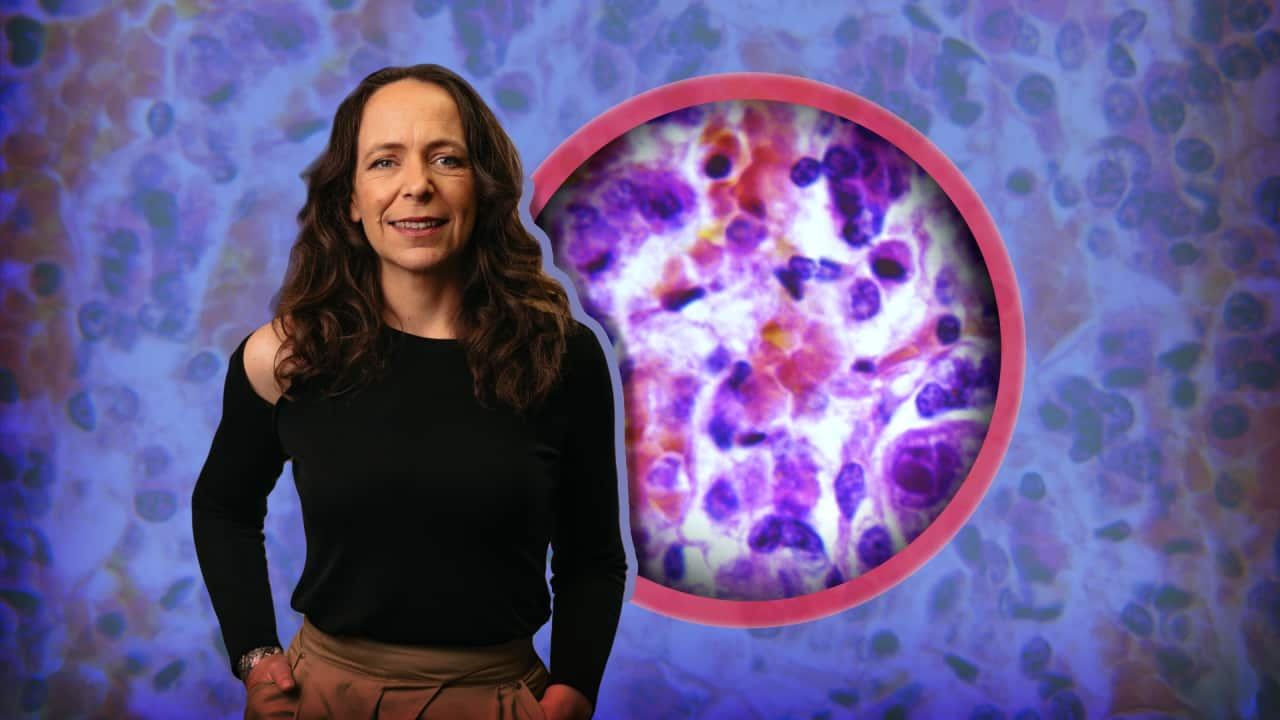
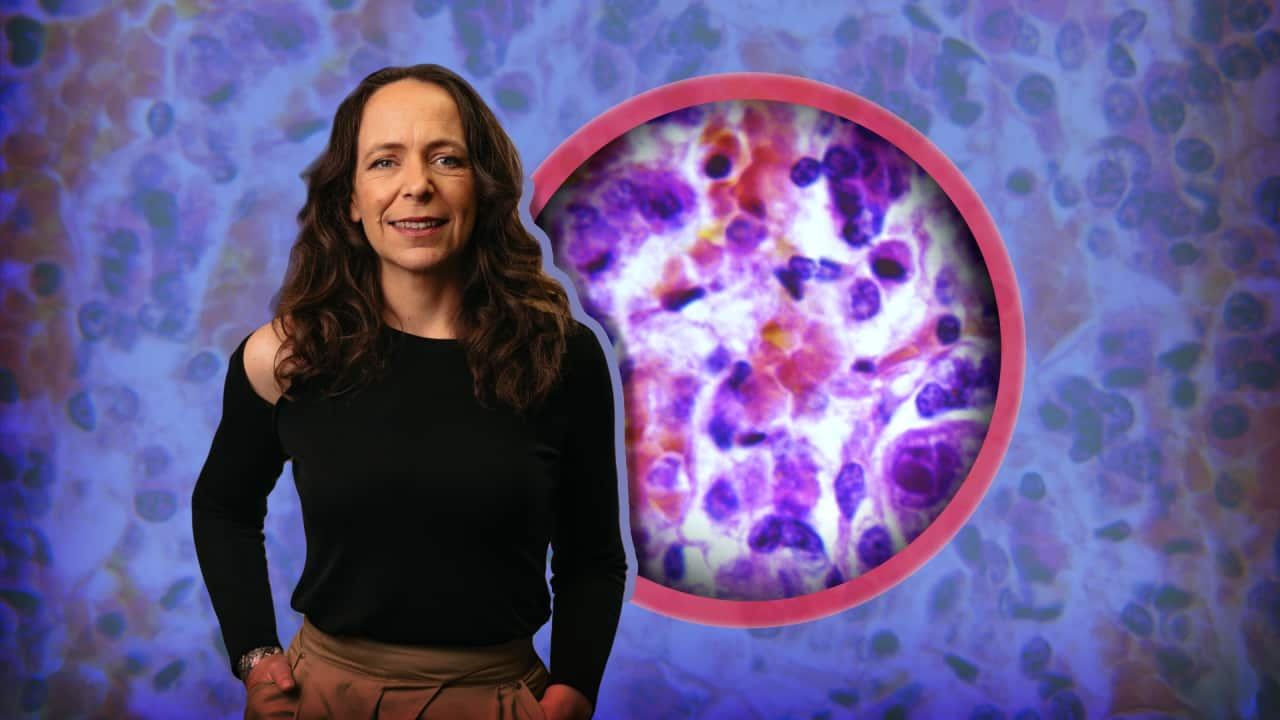
Dr Maud Eijkenboom says the current approach of developing new antibiotics is losing the battle to ever-evolving viruses and bacteria.
After her son struggled with an antibiotic-resistant disease, Eijkenboom set out on her own path to discover a better way to quell the rising wave of lethal pathogens.
In 2021, she founded Lixa, a Perth-based biotech company that has received international support for its "game-changing" research.
A decade of debilitation
Eijkenboom says her son Jonathan Barker once couldn't lead a normal life.
He was 12 years old when he started to faint regularly, and would fall asleep without being able to be roused — often for hours at a time.
"He virtually was a hundred per cent in bed," Eijkenboom tells SBS News.
"We had to carry him to the bathroom for two years, and then it took a total of six years to come back from it."
Barker had multiple infections stemming from Lyme disease, which he developed after being bitten by a tick in Europe. The disease is typically transmitted to humans by ticks carrying a bacterium called Borrelia burgdorferi. Scientists have not found the bacterium in ticks in Australia.
"It had become chronic, and it was pretty nasty, and it was very difficult to get to the bacteria [for analysis]," she says.
"My husband and I are both drug developers, and we looked around in frustration because we couldn't help our son."
That frustration propelled Eijkenboom and her husband to do their own research. They felt the medical world was too focused on developing new drugs and was not asking what could be done about antibiotics that were no longer working.
"Because we couldn't help Jonathan for a long time, we did a lot of research," Eijkenboom says.
After studying and working with university researchers, she raised capital and founded Lixa, aiming to find a solution to antibiotic resistance — for her son and others.
"You look around, and resistance and chronic conditions are everywhere," she says.
"You see elderly women with urinary tract infections, you see children with glue ear [a build-up of sticky fluid in the middle ear that can cause temporary hearing loss], there must be something in common across all bacteria that we need to be able to get to."
Rise of antimicrobial resistance
Antimicrobials are drugs such as antibiotics, antivirals, antifungals and antiparasitics that target and kill germs — or pathogens. These are microorganisms that cause disease and include bacteria, viruses, fungi and parasites.
The WHO has found that pathogens are developing antimicrobial resistance (AMR), making them harder to treat and causing patients to suffer through symptoms for longer.
Based on data from the National Antimicrobial Prescribing Survey, 50 per cent of Australian hospital patients will receive an antimicrobial, such as broad-spectrum antibiotics.
These are used to treat common infections, such as Neisseria gonorrhoeae, which causes gonorrhoea, and Methicillin-Resistant Staphylococcus Aureus (MRSA), which causes a range of skin infections as well as serious infections like pneumonia and sepsis.

Associate professor Rietie Venter, the head of microbiology at the University of South Australia, tells SBS News that AMR poses "significant treatment challenges".
"Pathogens can start showing signs of resistance to a new medication very fast, within a few years even," Venter says.
"Lower and middle-income countries often struggle with limited access to newer or last-line antibiotics, exacerbating the impact of resistant infections."
Venter explains that AMR is more than just a problem for wound care.
"The agriculture industry in the US, for instance, has a big problem with resistance, driven by the overuse of antibiotics in livestock production," she says.
Resistant bacteria can spread from farms into soil and water through animal waste, contaminating the food supply and surrounding environments, she explains.
AMR is even on the rise in households due to cross-contamination via washing machines and kitchen counters, which can harbour detergent-resistant germs.
"Supporting research and development of new antibiotics or alternative antimicrobial therapies is vital in combating the growing threat of antimicrobial resistance," she says.
An 'unconventional' new approach
Eijkenboom says her company's mission is to solve the antimicrobial resistance "crisis", not by creating new antibiotics, but by targeting the composition of deadly pathogens.
"We do that by breaking resistance. And we've got universal resistance breakers that tame bacteria," she explains.
"They go from a resistant state to a sensitive state, and suddenly the oldest antibiotics — or biocides or surfactants or whatever detergents you want to use — can work again as they used to."
The innovative approach neutralises pathogens and stops them from developing resistance to treatment. Pathogens typically develop resistance through genetic mutations, which are then passed on via rapid reproduction.
Some antimicrobials directly damage or disrupt the cell membrane, which is basically the bacteria’s skin.
When that happens, the cell leaks its contents and dies. But breaking it also triggers its survival instincts, allowing resistance to develop. So Eijkenboom’s approach is to avoid breaking the membrane.
"If you break the membrane of a bacterium, you create an evolutionary pressure, which will cause more resistance. So by not breaking it, you can bring back antibiotics again."
Lixa's technology has completed a phase one clinical trial using a nebuliser (a type of medical inhaler) to test its effectiveness in treating chronic respiratory infections.
She says it was found to be "very safe" for the lungs, one of the body's most sensitive organs.
The company is now looking to test an oral form, such as a tablet.
Lixa announced a partnership with the Global Antibiotic Research & Development Partnership (GARDP) on 2 February to scale the technology to market-readiness.
The GARDP is a not-for-profit global health organisation based in Switzerland that analysed Lixa's clinical data for 10 months before agreeing to support the company.
"Lixa's compounds represent an unconventional new approach to AMR treatment and after a review of their preclinical data, our experts thought that it is worth supporting Lixa to generate additional data to pressure-test their approach," François Franceschi, an associate director at GARDP, said in a statement.
"If their technology is found to be safe and effective in clinical trials, this could represent a game-changer in the way we treat drug-resistant bacterial infections."
The innovation gap
James Graham, the CEO of Recce Pharmaceuticals, says "next-generation novel approaches are urgently needed to stay ahead of this crisis".
He tells SBS News there is an "innovation gap" where a lack of funding and resources means new medicines are hard to research and develop.
"Most antibiotic classes we rely on today were discovered between the 1940s and 1980s, and no new class has been approved in over 40 years," he says.
Recce Pharmaceuticals, a biotechnology company headquartered in Sydney, is developing a new product designed to combat AMR: synthetic anti-infectives.
Graham says that while this kind of innovation is very much needed, the process of researching, trialling and taking a new treatment to market in Australia is long and expensive.
"We've spent nearly $100 million getting this new class of antibiotics into a late-stage phase three trial," he says.
"And we're not done yet."
Clinical trials typically consist of three phases, says Graham, covering discovery through to testing in labs and, finally, in people.
"The final piece of that is at the end of phase three, you obviously then submit for market application, which can take many months to about a year."
Graham says more financial investment is needed in companies looking for solutions to AMR, but he believes Australia is "really well placed" to support new innovation.
He describes the federal government's research and development tax incentive scheme as an "incredibly compelling" program, which can enable companies to offset R&D expenditure up to $150 million. Those with an annual turnover of less than $20 million can offset costs equal to their corporate tax rate, plus a premium of 18.5 per cent. The premium is lower for companies with higher turnover.
"That's incredibly unique anywhere in the world. So if you're in the United States, you're lucky to get 2 to 5 per cent [of expenditure offset]," he says.
'Create a life now'
Eijkenboom says her son, who is now 22, can leave the house again.
"It took 10 years for him to recover; he didn't have any schooling, no high school, because he was asleep," she says.
"When we count the impact of AMR, we count the people who die, but we don't count the people who are debilitated, who can't take part in a normal life."
She says her son is "much better now" and found his first job a few months ago.
"He doesn't want to look back on his illness. And he just wants to go ahead and create his life now."
Eijkenboom is looking to the future too. She believes Lixa’s work, although in its early stages, could make a unique contribution to the fight against AMR.
"I think we're onto something and that we're really kicking some big goals, and it's quite interesting to do that from little Perth, whereas the rest of the world is still stuck in developing antibiotics."
For the latest from SBS News, download our app and subscribe to our newsletter.





