Listen to Australian and world news, and follow trending topics with SBS News Podcasts.
TRANSCRIPT
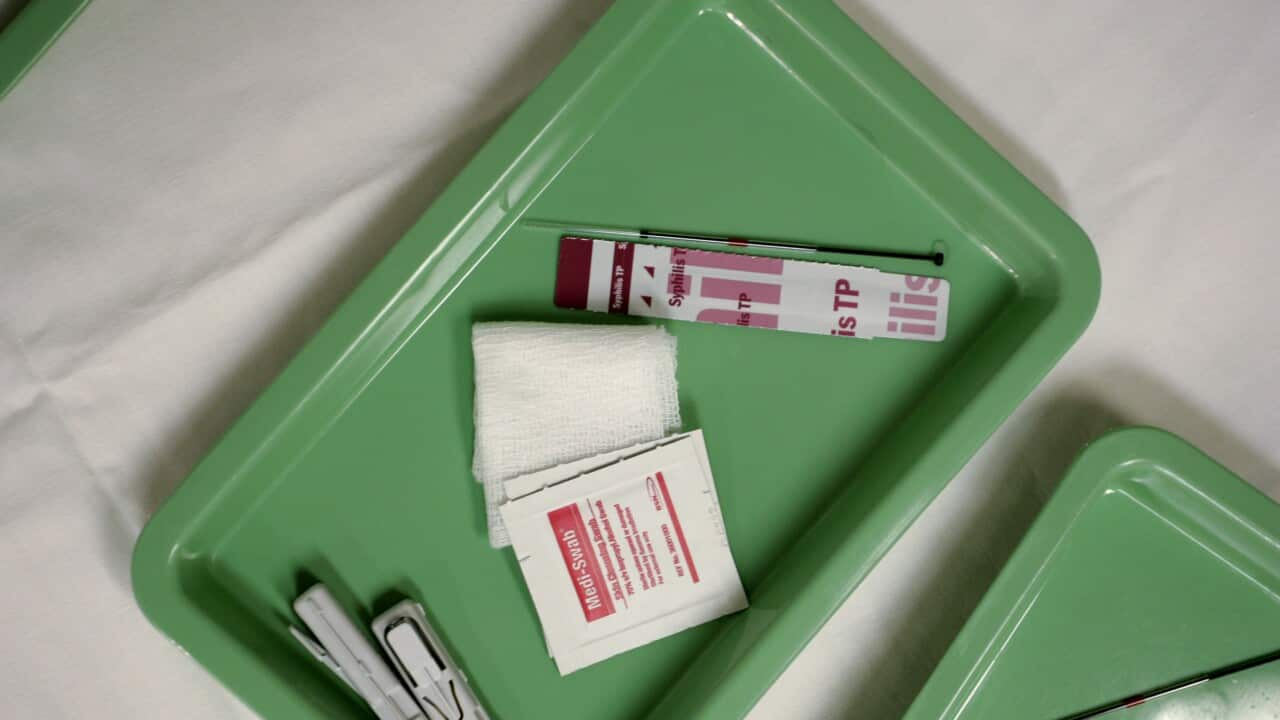
Experts say syphilis and gonorrhoea are easily treatable and preventable.
But in Australia, infection rates have roughly doubled over the past decade.
This message from Dr Skye McGregor, an epidemiologist at the Kirby Institute.
"A prevention approach really is around having discussions around sexual health with your partner, regular testing, timely treatment ... Condom use of course is also important, it can prevent a significant proportion of STIs."
Last year, there were nearly 6,000 diagnoses of syphilis, according to a new report from the University of New South Wales' Kirby Institute.
While most cases are still in men, infections in women have quadrupled over the past decade.
There were also more than 44,000 diagnoses of gonorrhoea last year.
And chlamydia remains the country's most diagnosed S-I, with nearly 102,000 cases in 2024 – around half of which were among people aged 20 to 29 years.
"While we haven't seen much change in the numbers, what we'd like to see is that starting to come down.
Cases of HIV have actually dropped over the past decade with more than 750 cases recorded last year – 62 per cent attributable to sex between men.
Doctors say preventative medications have helped, but there still needs to be vigilance for other STIs.
What has experts really alarmed, though, is the rate of congenital syphilis.
Dr McGregor says it has resulted in 34 infant deaths, recorded over the past decade.
"In pregnancy untreated syphilis can lead to miscarriage, still birth, congenital syphilis – which can result in life long disability – and death of infants, so it's a serious and entirely preventable outcome."
More of than half of those deaths were among First Nations people.
Rates of gonorrhoea, syphilis and chlamydia were also 2 to 5 times higher among the group.
Robert Monaghan, the Kirby Institute's inaugural Manager of First Nations Health Research, says those figures are deeply alarming.
"I think a lot of that is about access – access to services – and timely diagnosis and treatment. That is one of the biggest problems we see, especially more so in our remote Aboriginal communities. It's about choice as well. In most Aboriginal communities, especially remote, you only have one choice – which is mostly the Aboriginal Community Controlled Health Service – which do a marvellous job but they're under capacity."
The snapshot offered by the report suggests only 16 per cent of people aged 16 to 49 have been tested for an STI.
There are efforts towards improving rates and stigma, including self-testing kits and STI tele-health appointments.
But Dr McGregor says more needs to be done.
"We do know that it points to persistent inequities in testing and prevention and healthcare. And certainly that's where we need to focus our efforts to understand who's missing out on testing. If we look, for example, at the congenital syphilis data, we know for mothers who have had infants with congenital syphilis, the majority of those didn't receive testing early in their pregnancy. So, we need to work with the communities most impacted to understand what are the programs contribute to reduction in all of these infections."
That approach, Robert Monaghan says, is also intended to breakdown stigma and shame.
"We need a wider depth of health promotion in our schools that start that early conversation that take the stigma away from it because people are educated on it. We see the education around STIs and BBVs (Blood-Borne Viruses) is declining in these areas. Programs going into communities need to be co-designed they need to have ownership from our Aboriginal communities – and that is the best outcome."