Deborah Olle had “peace of mind” when she got the all clear from a bowel cancer screening test she did when she was 60. Her two previous 'poo tests' at age 50 and 55 had also returned negative results.
But less than a year after the third all clear, Ms Olle went to her GP, suffering from indigestion. The GP sent her for an endoscopy, suggesting she also have a colonoscopy because “you may as well, while you’re under.”
While the endoscopy found a stomach ulcer which was easily treated with antibiotics, the colonoscopy revealed something far more sinister.
“I had two sessile serrated polyps which are flat polyps and they’re very hard to find,” Ms Olle, 62, told Insight. “I had no symptoms, none at all.”
“Underneath one polyp was an ulcer, five millimetres in diameter, and it had dropped into the mucosal layer (of my bowel) by less than half a millimetre, and that cost me a third of my colon.”
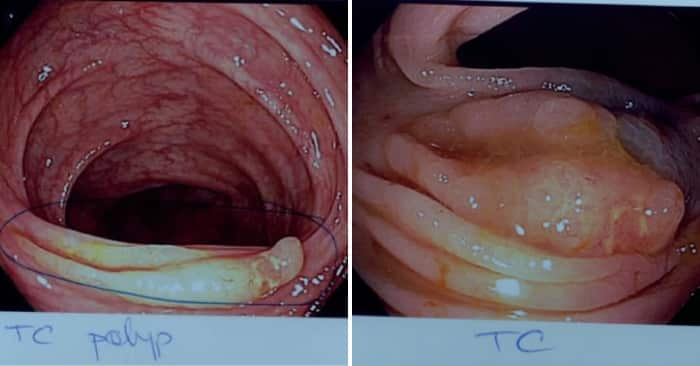
The polyp was ulcerated, and had invaded the mucosal lining of Deborah's bowel. Source: Supplied
Ms Olle had major bowel resection surgery as a result. “Even though the (cancerous) polyp was tiny, the only option was still a very large operation,” she said.
“I did not need a colostomy bag or chemotherapy, or radiation, but I do have problems every single day of my life with diarrhoea.”
From this year, all Australians aged 50 – 74 will receive a free 'poo test' in the mail every two years to screen for bowel cancer. The test aims to detect microscopic blood in the stool which could indicate the presence of polyps, even before they are cancerous. A positive ‘poo test’ result warrants further investigation by colonoscopy, but only three to four per cent of cases are found to have cancer.
“If you’re negative on a poo test, your chance of being diagnosed with bowel cancer before the next test comes in two years is less than one in a thousand,” Dr Cameron Bell, a gastroenterologist from Sydney’s Royal North Shore Hospital, told Insight.
“It’s overall a very reliable test.”
We know that some [colonoscopists] find zero per cent of [sessile serrated adenomas]. So don’t go to them. Just go somewhere else.
But the type of polyp which Deborah Olle had is undetectable by the test because flat, sessile serrated, adenomas don’t bleed.
“These are the bad guys on the block," Dr Bell explained.
“They’re hard to find at colonoscopy, but the Faecal Occult Blood 'poo test' is even less reliable [in finding these type of polyps].
"There was probably no occult blood to find, and when [Deborah] had the test, the polyps were probably still benign and changed rapidly.”
He advised people to be vigilant when choosing a colonoscopist and to always ask if the specialist has been recertified, because “the quality of colonoscopy from colonoscopist to colonoscopist varies enormously.”
“We know that some people find zero per cent of these (sessile serrated adenomas). So don’t go to them. Just go somewhere else,” Dr Bell said.
While bowel cancer is Australia’s second biggest cancer killer after lung cancer, it is largely preventable through screening and healthy lifestyle changes, and it’s 90 per cent successfully treated if found early.
Yet, the Australian Institute of Health and Welfare says only 41 per cent of people who receive the ‘poo test’ kit actually do it. It’s predicted that if that participation rate increased to 60 per cent, around 84,000 lives could be saved by 2040.


