Listen to Australian and world news, and follow trending topics with SBS News Podcasts.
TRANSCRIPT
When GP Melanie Mapleson noticed a lump above her collarbone, she went and got it checked immediately and waited for her results.
"Those days prior to the diagnosis when I'd felt the symptoms but hadn't got any answers, they were some of the worst days of my life".
As a doctor herself, the 38-year-old knew there could be something seriously wrong, and what she was diagnosed with shocked her.
“My mind was jumping to the worst possible case scenario and the worst conclusions, even though they were all hypothetical at that stage. So everything stopped. I stopped working. I basically just went into - sort of withdrew into - a state of numbness and just got all the necessary investigations and then was told by my lovely GP that I had Hodgkin's lymphoma.”
After being diagnosed with cancer, Ms Mapleson heard about radiotherapy as a treatment option, but she was worried about potential side effects.
“You go on deep dives when you're diagnosed with something like this, it's hard to resist the temptation to go and look at every possible source of information, even those that are most unreliable. And so it wasn't so much the team that was giving me misinformation, they were very clear on the fact that the radiotherapy would be a critical integral component of my cure. But some of the information that I was channelling through was incorrect. And I think that's where my fear was based, you know, around side effects and late effects and being radioactive. And I had a young child, so I was afraid of putting him at risk and all of that was really completely non-factual, but that's what the mind settled on when you're in a place of uncertainty and fear.”
Ms Mapleson decided to go ahead with radiation therapy as part of her treatment.
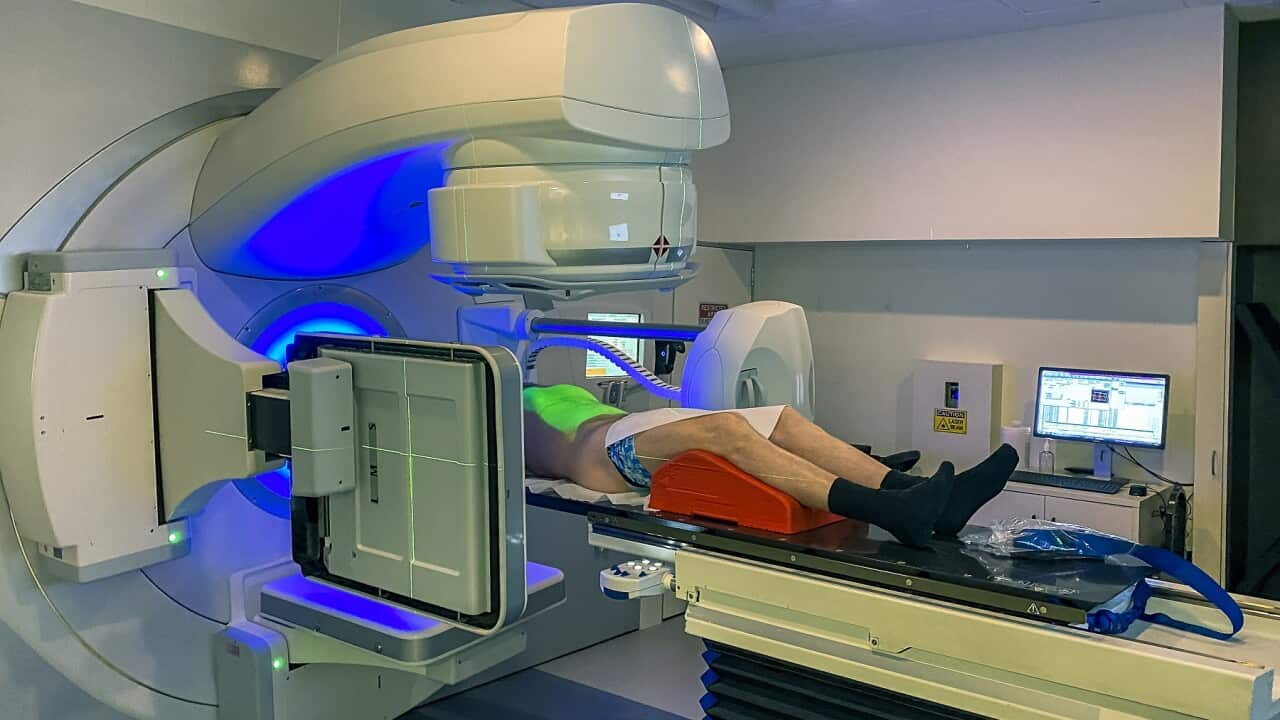
“I turned up, got changed, lay down on the examination bed, and then was there for about 10, 15 minutes just lying there very, very still. And then I left. So there was really not much to it, and the staff were really lovely and receiving the radiation therapy, was never painful. I wasn't radioactive and my skin didn't break down and I didn't lose hair or anything based on the radiotherapy. So I had a bit of a mild cough for a period of time and some sensation of I guess discomfort while swallowing. But that was very short-lived. And because I was expecting it, I knew that it was part of that immediate side effects from the treatment that I'd had, and it did go away just as they said it would. So that was really it.”
Professor Sandra Turner, a senior radiation oncologist at the Sydney West Radiation Oncology Network at Westmead Hospital, says there are a lot of misconceptions when it comes to radiotherapy.
“I think the common things we hear are that people fear radiotherapy and they worry that it's going to cause damage and side effects. They don't understand how safe and sophisticated it is. Often people think that you are going to be radioactive when you have treatment and that could be damaging to people's families or children or pregnant people. And although there are some much less common forms of radiation therapy that use radioactivity, the vast majority of people having radiotherapy are never radioactive. And the other thing is that people get very confused between chemotherapy and radiotherapy. So they don't understand that radiation is very focused, only treats the area that we need to treat with a very narrow safety margin. And so a lot of those generalized side effects like nausea and vomiting and other things that you can get from chemotherapy are much less common with radiotherapy, depending on that part of the body that we are treating.”
Professor Turner said that despite being a long-standing cancer treatment, 1 in 5 Australians who need radiotherapy never receive it. Research shows that people can be referred late which can reduce the treatment's effectiveness. There are also few to no radiotherapy machines in some parts of regional and rural Australia.
“We know that sometimes lives can be lost because people don't get radiotherapy when they should. So we feel very much that every health professional, but particularly every doctor, needs to know at least the basics about what radiotherapy can do, how safe it is, how sophisticated it is, and what the process is of delivery so they can help advise and refer their patients like they need to on a whole lot of medical issues.”
She explained that the technology has improved immensely over the last few decades and now contributes to at least 40 per cent of cancer cures.
“There used to be some places in the body that we couldn't easily use radiotherapy because of the sensitive structures or organs next to that area. And we are now able with our new technologies to be able to get around those problems. And mainly this has come about through being able to accurately visualize the organ or part of the body that's being treated at the time it's being treated. We can even follow where the cancer is within the target area that we are treating. For instance, in organs like say the lung, which moves a lot as people breathe when we're delivering the treatment, we can now make sure that we compensate for movement so that we can accurately track, for instance, the cancer in the lung so that we can be sure we're treating it every second that the machine is turned on.”
One type of cancer where radiotherapy is particularly effective is prostate cancer.
Kuldeep Duhan was diagnosed with the illness two years ago, he decided to go with radiotherapy treatment after hearing his options from oncologists.
“It was an easy decision for me to do it because if I went for the surgery I would've had to take a month off. And from a work point of view, it won't suit me. When you are getting the radiotherapy done, you don't feel anything and everything was really seamless from my point of view. Basically I continued to work because I'll get it done in the morning and then come to work and I'll do my normal days work.”
The 63-year-old goes for regular check-ups and is grateful to his care team for the support he receives, while Ms Mapleson has reached two years of complete clinical remission.
Professor Jared Martin, a clinical and research radiation oncologist, said radiation therapy is an effective cancer treatment, but that it's often best used in combination with chemotherapy and surgery.
“A lot of what we've learned from clinical trials has often been for some quite complex cancers which that just one treatment alone is unlikely to get the best outcome. Quite often you do need to get some combination of both or even all three of those modalities in a very particular kind of sequence and even overlapping sometimes to get the best chance of controlling the disease. And then on top of that, we obviously also try to prioritize quality of life because the side effects both from the tumour as well as the treatment are a huge factor. And when we have shared decision making with patients, we really do try to be very collaborative, I guess, on trying to figure out priorities, because for instance, I treat a lot of prostate cancer and it might be for a particular couple, sexual function might be a huge priority and that might be very important in helping guide treatment decisions.”
Professor Martin said while research into radiotherapy has been revolutionary, there has been poor messaging around its benefits, which extend beyond cancer.
“This is kind of a bit mind-blowing, but it actually turns out that very low dose radiotherapy may be of some benefit for people with some chronic inflammatory conditions like plantar fasciitis, for instance, which is a condition that can affect people's ability to walk. So in radiation oncology, we're now working hard to get good high quality data about exactly how much we can maybe help people with these other conditions as well.”
Professor Turner is also the co-chair of World Radiotherapy Awareness Day, being launched on the 7th of September.
“World Radiotherapy Awareness Day is a way to bring the whole radiation oncology community together, and also people that have been touched by cancer and had radiation therapy, patients and survivors, and their families, and bring everyone together to raise their voice around the same issues that are worldwide. And these are about lack of awareness, lack of education, fear of radiotherapy, and access to radiotherapy, because we haven't talked about this, but in many places in the world, there aren't even any radiation machines. And ultimately, what we'd like to do is to use that joint power and amplification of that voice to impact decision makers, policy makers, and governments to understand the importance of radiation therapy and to appropriately invest in radiotherapy services that are needed to make sure that all patients get good access to radiotherapy.”
Organisers of World Radiotherapy Awareness Day says research shows that over 200 million people live in a country with no radiotherapy facility.