Indigenous health professionals say calls to adequately fund oral healthcare in Australia are nothing new.
In a country that has a universal health scheme in Medicare, it has dumbfounded many that the same safety net does not exist for the one part of our body we use the most every day: our mouth and teeth.
The gap in oral healthcare is particularly concerning for Aboriginal and Torres Strait Islander people: the rates of gum and dental disease are higher, and there remain barriers to accessing dentists, despite many people being eligible for some work either through mainstream public dental clinics, or Aboriginal medical services.
That gap was pulled into sharp focus in early April as the coronavirus pandemic meant all except emergency procedures had to be deferred.
Those restrictions have begun to ease, but the CEO of the peak body for Aboriginal medical services, Pat Turner, told NITV News on Tuesday that the oral health gap remains.
“Oral health has always been an area underfunded for our people,” Ms Turner told NITV News.
“If you’re in Sydney at the moment, the Redfern [Aboriginal Medical Service] dental clinic is closed and people with emergencies are being referred to the Sydney dental clinic.
“We are very concerned that overall our ability to provide a full dental service to our people is totally underfunded."
Flying overseas for dental care
There are around half a million people on waiting lists for dental care across the country, but in the public health system many procedures won’t be covered due to budgetary constraints.
When Adam Manovic went to a dentist in 2016 he was told if he didn’t address his gum and dental health within a year, his teeth would fall out.
“That scared me,” he said.
“My daughter Rosie had just been born, and I thought she would never know me with teeth. I never knew my mum with teeth.”
Mr Manovic was knocked back by the Aboriginal Medical Service for the work he required and quoted up to $32,000 by private practices.
He opted to get his teeth fixed in Thailand for a fraction of the price.
“I’m never going to go to the dentist in Australia ever again. The service was so good, and it was a reasonable cost,” Mr Manovic said.
While that experience is increasingly common, health professionals have warned against going overseas where Australia’s strict health standards might not be followed.
Naming the barrier
As leading health bodies fight for universal dental care, Australia’s first Indigenous dentist, Dr Chris Bourke, said focusing on prevention is just as important.
One of the keys to good oral hygiene, he said, is access to a clean, quality water supply – and other healthy alternatives to sugary drinks.
But the drought in western New South Wales has seen places like Walgett resort to trucking in bottled water, while communities in Queensland and the Northern Territory have continually voiced concerns over the quality of their groundwater.
“We know... that up until 2012 in Queensland, 90 per cent of towns and communities had a fluoridated water supply,” Dr Bourke said.
“Because of a change of government in the 2012 election, that's gone back to 76 [per cent]… because Aboriginal and Torres Strait Islander people are more likely to live in those areas where there is no fluoride, nearly 50 per cent of Queensland's Aboriginal and Torres Strait Islander people have no fluoridated water supply.
“This means that they suffer higher disease levels.”
Increasing the number of Indigenous dentists and addressing institutional racism is another area Mr Bourke said we need to focus on.
There are currently just over 100 Indigenous dental health professionals in Australia, and if that number goes up – according to Dr Bourke - then so too does the cultural safety of many Indigenous patients.
“There's a substantial power differential when you're going to see the dentist,” he said.
“Dentists and dental practitioners need to be able to recognise that. Particularly when they're dealing with Aboriginal and Torres Strait Islander people who had long histories in this country of being very badly treated by people in authority.
“That results in people feeling like they're being talked down to or disregarded, or what they really want is not being listened to or understood.”
Social Barriers
Shanell Morgan is 36 years old and – in addition to having less than 10 teeth remaining – she has a crippling fear of the dentist.
Ms Morgan told her story as part of an SBS Insight special into the Dental Gap.
Ms Morgan said she requires work that costs around $8,000 but the only way she can see a dentist is if she is put to sleep during the procedure – a cost not usually covered by the public system.
“We need more opportunities for people with a fear to go under and put to sleep to get teeth done, because that’s the only way it’s going to happen for people like myself.
“Waiting lists are way too long. Right now I’m not even on a list.”
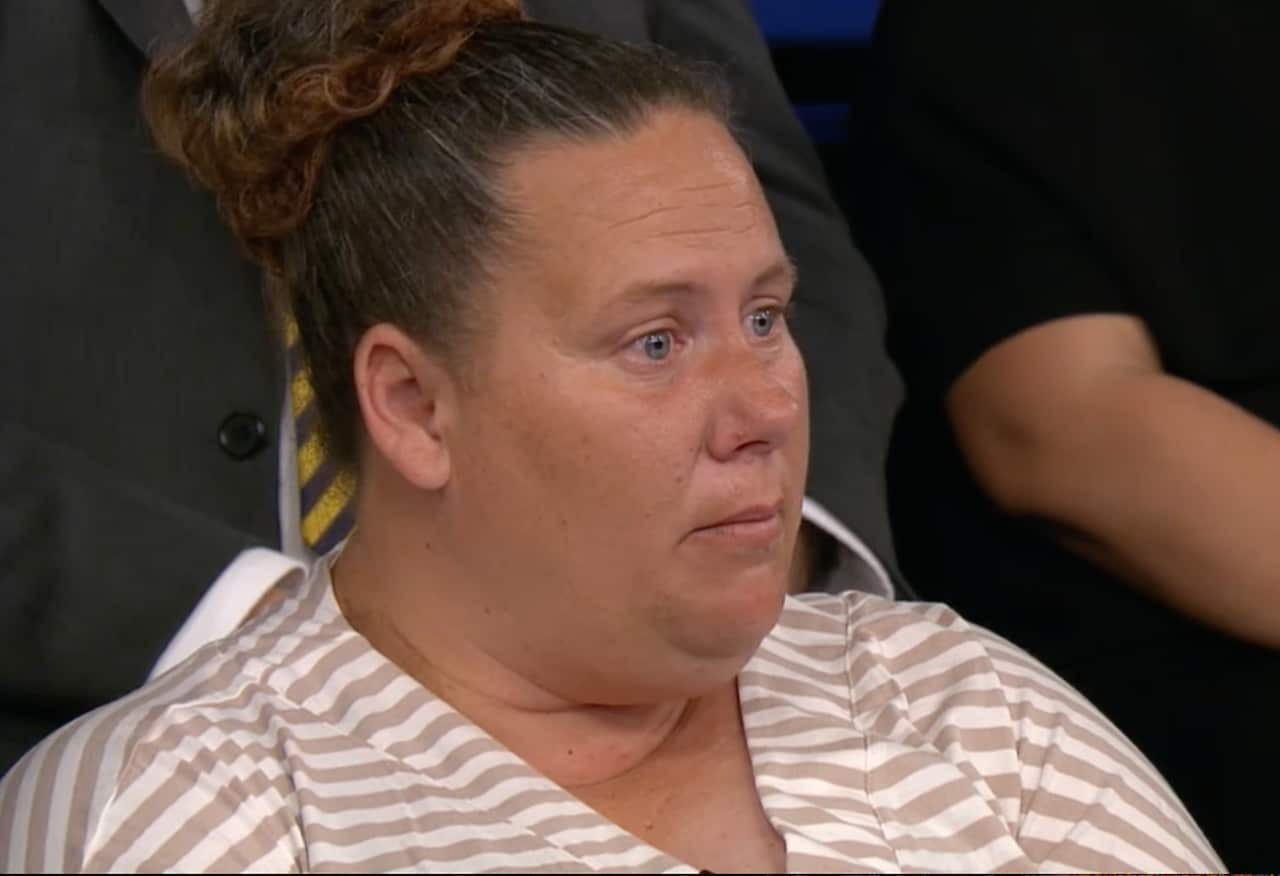
Ms Morgan said she has never taken a photo with her 7-year-old son and struggles to leave the house.
It’s a reality Dr Bourke said many people live with.
“The social impact of a poor appearance arising from bad teeth is really something that we need to fully understand and really do something about it,” he said.
‘One of the gaps that needs to be closed’
Meanwhile Ms Turner said funding a full dental service that Aboriginal Health Organisations can provide would go a long way to closing the gap.
“It is totally unacceptable because we have massive oral health issues right across the spectrum no matter where our people live,” she said.
“And this is one of the gaps that needs to be closed as we move forward in terms of direct funding to our sector to ensure timely preventive and dental work is available and readily accessible to our people.”
Mr Manovic said receiving the dental care he required overseas has changed his life.
“Its done so much for my confidence, I didn’t smile much in photos before that, which was bizarre. Now I do.”
Insight:The Dental Gap will air on SBS at 8:30pm Tuesday night.

